With Covid-19 hospitalizations steadily approaching a document excessive within the US, states like Arizona have activated emergency plans and r
With Covid-19 hospitalizations steadily approaching a document excessive within the US, states like Arizona have activated emergency plans and requested refrigerated vehicles to arrange for overflow at morgues. Medical doctors there say packed emergency rooms and ICUs are forcing them to prioritize the sickest sufferers, leaving different in poor health sufferers to deteriorate whereas ready for care they’d ordinarily obtain instantly.
Hospitals in sizzling spots throughout the nation are increasing and even maxing out their workers, tools, and beds, with docs warning that the worst-case situation of hospital assets being overwhelmed is on the horizon if their states don’t get higher management of the coronavirus.
“With Covid, lots of occasions individuals who aren’t sick sufficient but get pushed to the again, after which they will develop into actually, actually sick sadly as a result of we had been focusing our efforts on the people who find themselves getting ready to loss of life,” an emergency room physician on the Banner Well being system within the Phoenix metro space, who requested to go unnamed fearing retaliation from his employer, advised Vox.
Different docs in Arizona, the place 88 p.c of hospital beds statewide had been in use Tuesday, say the shortage of assets means they’ll quickly be rationing medical care, as docs in Italy had been compelled to do.
“The worry is we’re going to have to begin sharing ventilators, or we’re gonna have to begin saying, ‘you get a vent, you don’t.’ I’d be actually stunned if in a pair weeks we didn’t have to do this,” says Murtaza Akhter, an emergency drugs doctor at Valleywise Well being Medical Heart in Phoenix.
It’s not simply Arizona. Medical doctors and hospital consultants in Texas and Southern California say capability is a serious concern for them as nicely, notably if new day by day circumstances preserve rising. A number of counties in Southern California are additionally now going through main outbreaks of the virus, with hospital assets stretched skinny to look after the sickest sufferers.
States have began to roll again their reopenings in recognition of the severity of present transmission. California Gov. Gavin Newsom introduced Monday he would order some companies to shut once more. Texas Gov. Greg Abbott has lastly issued a statewide masks mandate and in addition closed sure institutions. Arizona Gov. Doug Ducey additionally reimposed some restrictions, although has refused to require residents to put on masks in public areas, as an alternative asking for voluntary compliance with public well being consultants’ recommendation.
The query is, will or not it’s sufficient?
“If issues proceed to worsen,” John Swartzberg, a medical professor emeritus at UC Berkeley’s Faculty of Public Well being, says, medical look after Covid-19 sufferers “will get rather more draconian.”
When New York and New Jersey raced to develop hospital capability in April to deal with the crush of Covid-19 sufferers, Solar Belt states largely prevented the massive spring wave. However after their governors moved ahead with reopening in Could regardless that they didn’t meet the general public well being standards set by the federal authorities to remain secure, three states specifically — Arizona, Texas, and Florida — noticed important will increase in new circumstances.
Specialists say these outbreaks are largely pushed by individuals flocking to newly reopened eating places, bars, gyms, and different high-risk indoor areas, in addition to weakly enforced or nonexistent face masks mandates. Now, with new circumstances and hospitalizations rising in 44 US states and territories, many worry some sizzling spots could also be confronted with even larger surges, with much less capacity to develop capability than hospital-dense New York Metropolis.
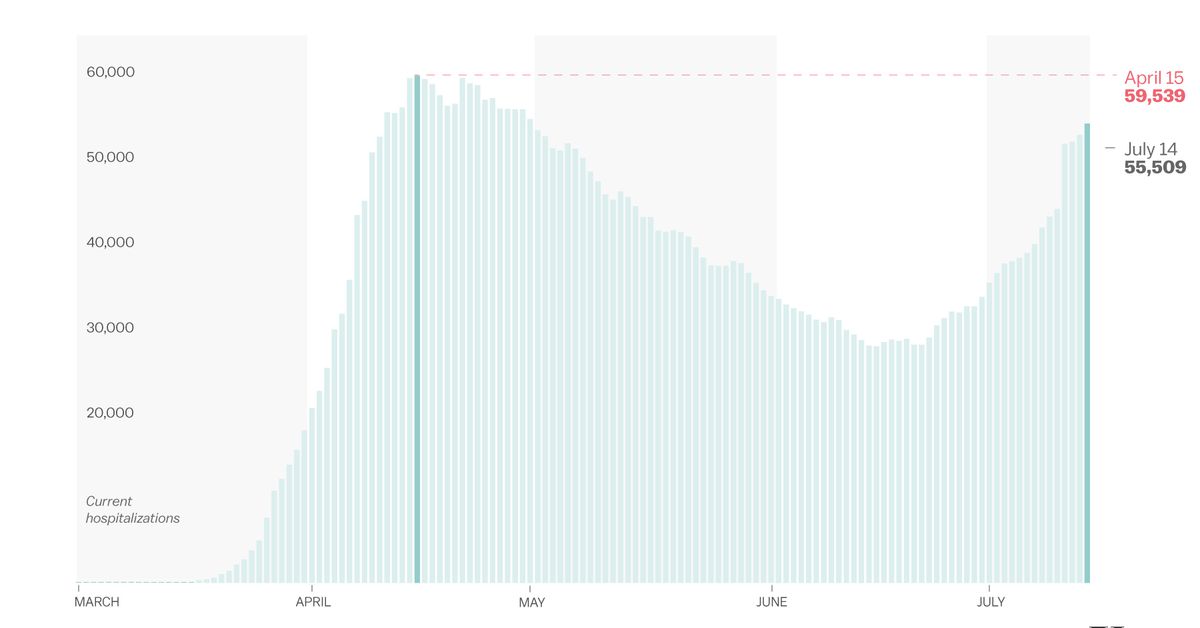
Hospitalizations nationwide are actually rapidly on their strategy to exceeding the height of 59,539 on April 15, hitting 55,509 on Wednesday, in keeping with the Covid Monitoring Venture.
:no_upscale()/cdn.vox-cdn.com/uploads/chorus_asset/file/20085577/second_wave_hospital_chart.jpg)
Christina Animashaun/Vox
Hospital organizations in Florida say services there can nonetheless develop capability if wanted. However they, like different sizzling spot hospitals, are beginning to reduce on elective surgical procedures and procedures — main them to furlough workers in some circumstances to compensate for enormous losses in income — to accommodate the rising tide of Covid-19 sufferers.
And most worrying for the states now battling main outbreaks is that, in contrast to in April, when many of the nation was in lockdown, there’s no clear sense of when the present outbreaks will peak or decline. With solely partial social distancing measures in place and inconsistent masks use, the virus could proceed to unfold, resulting in an unabated wave of extreme sickness requiring hospitalization, extra deaths, and extra long-term issues requiring medical care.
Right here’s a better take a look at how some hospitals in Arizona, Florida, Texas, and Southern California are dealing with the pressures of the newest surge of Covid-19 sufferers, and why it could worsen within the coming weeks.
Arizona docs say the surge is forcing them to make brutal choices in affected person care. In the meantime, morale is dangerously low.
As Vox’s German Lopez has reported, Arizona’s Covid-19 outbreak has these days been the worst within the nation, with the very best check positivity fee of all of the states: 24.7 p.c of exams coming again optimistic (practically 5 occasions the advisable most of 5 p.c), in contrast with 18.7 p.c in Florida and 17 p.c in Texas, in keeping with Johns Hopkins.
It additionally, till very lately, had the very best variety of day by day circumstances per 100,000 individuals. (As of Wednesday, Florida was within the lead, with 54 new circumstances per day per 100,000 individuals, in contrast with Arizona’s 48, in keeping with knowledge compiled by the Washington Put up.)
Whichever metric you’re taking a look at, the implication is identical: The virus continues to unfold quickly within the state, regardless of the governor’s (comparatively weak) efforts to discourage indoor gatherings and guarantee widespread face masks use since reopening. In the meantime, hospitalizations are rising steeply following the upward pattern in new circumstances. The warmth wave underway, which is forcing extra individuals indoors, isn’t serving to, both.
The unchecked transmission of the virus within the state and ensuing strain on hospitals are notably infuriating to some emergency room and ICU workers, who say they’re dropping hope that they’ll get any aid from the surge of severely in poor health Covid-19 sufferers anytime quickly. They usually’re having to make choices on the fly they’re uncomfortable making.
“Sending individuals with Covid house with oxygen tanks as a result of we don’t have the assets for them?” says Akhter of Valleywise Well being. “That is one thing I’ve by no means carried out in my life earlier than. That is loopy. And that is gonna be even worse in a few weeks. Up to now we’re making an attempt to carry regular, however how lengthy will that final?”
The psychological toll, he says, is severe too.
“To return off a shift and be like, ‘I’m dropping hope’ — that’s a harmful place to be in,” he says. “I don’t wish to really feel that means. And that’s as a result of regardless of the horrible numbers, regardless of the actual fact I’m nonetheless getting the Covid circumstances [in the ER], regardless of what we’ve been saying to the media from the entrance line, I drive house from work and I actually see a number of individuals congregating collectively intently and within the grocery retailer not carrying masks.”
One other ICU physician in Phoenix, who requested anonymity as a result of his employer has forbidden workers to talk to the media, described more and more low morale amongst well being care employees within the state.
“I believe lots of us really feel as if our group has deserted us virtually, as a result of there’s lots of faux information about how masks aren’t serving to the unfold,” he says. “I believe there’s only a sense of abandonment virtually the place we really feel like we don’t have the help of our group; this particular person selfishness that we’re seeing in society is de facto upsetting. And I believe psychologically it’s actually affecting lots of my nurses and workers.” A few of them, he says, are so annoyed and fearful about getting sick themselves that they’re not coming to work as a lot, calling in sick, or simply chopping their hours.
Akhter believes there are lots of people in Arizona who nonetheless don’t imagine Covid-19 is unhealthy. “If their mom will get sick, even with non-Covid, with appendicitis, for instance, what do they suppose goes to occur if there are not any hospital beds? I don’t know what else to say apart from like, ‘What if your beloved will get sick, the place do you suppose she’s gonna go?’”
A few of his colleagues in emergency and demanding care drugs say they’re already working out of ICU beds. “We’ve got sufferers who’re admitted to the ICU, however there isn’t a bodily ICU mattress for them,” says the ER physician at Banner Well being who requested to not be named. “So that they bodily keep within the ER. They usually have been staying within the ER for over 24 hours as a result of there may be nowhere else for these sufferers to go. After which we’re utilizing ventilators which have beforehand been retired, which can be extra more likely to trigger lung damage on sufferers, as a result of, once more, there’s no different choice, no different means.”
The crunch on beds is getting so tight that Tucson Mayor Regina Romero lately advised CNN that Pima County might need to ship sufferers to different states for care. “Any day, we’re going to need to be sending sufferers to different states due to our lack of capability,” she says.
Banner Well being system, the biggest hospital community within the state, says it has been capable of develop capability to date to maintain up with the heightened demand from Covid-19 sufferers, transferring them and assets between hospitals to maintain volumes balanced and manageable. In latest weeks, it has additionally introduced in about 400 journey nurses and respiratory therapists from out of state, spokeswoman Becky Armendariz advised Vox over electronic mail. However she didn’t rule out the potential of exceeding capability. “It’s actually doable for us to achieve max capability if the pattern in circumstances continues.”
The one strategy to keep away from that at this level, the docs say, is for extra individuals to begin carrying face masks and for officers to implement mandates on the metropolis stage.
“If Arizona doesn’t masks up, we’re in massive, massive bother,” says the ICU physician. “That’s the bottom actuality of the state of affairs.”
Florida hospitals are strolling a path “with a precipice on both facet”
By way of sheer numbers of recent circumstances, Florida — the third most populous state within the nation — has persistently been within the lead this summer time, with a document excessive of 15,300 new day by day circumstances on Saturday. (On Tuesday, the variety of new day by day circumstances fell to 10,101.) Greater than 4,400 Floridians have died because of the virus, with a median of 81 deaths per day in latest weeks.
In accordance with Justin Senior, CEO of the Security Web Hospital Alliance of Florida, which advocates on behalf of 14 hospitals within the state that present care no matter sufferers’ capacity to pay, the state’s hospital capability has not been reached but and there’ll nonetheless be many hospital and ICU beds accessible if hospitalizations proceed to rise quickly.
Even so, Senior says hospitals are in a precarious place, “with a precipice on both facet” as they attempt to juggle the wants of non-Covid-19 sufferers with the rising variety of Covid-19 sufferers. In the event that they postpone elective procedures, like sure surgical procedures, they lose income at a time once they’re nonetheless reeling from dropping, by his estimate, $5 billion to $6 billion total from March to Could when the state shut down. In the event that they don’t postpone these procedures, it’s more durable to look after sufferers in a Covid-19 surge, he says.
“That is the trail that the hospitals try to stroll, since you don’t need one other shutdown fully when there aren’t sufficient sufferers to keep away from layoffs and keep away from a very unhealthy monetary state of affairs on one facet, and naturally, overcapacity and overtaxing of assets with too many Covid sufferers on the opposite facet,” he says.
In Florida, Senior says, workers is the most important concern for hospitals in the mean time — specifically ensuring that they don’t burn out and have sufficient PPE to remain protected against the coronavirus. “This can be a actually disturbing state of affairs and there’s an actual recognition of that.”
In accordance with CBS Native in Miami, Florida Gov. Ron DeSantis has requested that the Federal Emergency Administration Company (FEMA) ship 1,500 nurses to the state to alleviate the strain on overworked hospital workers. “As of Monday morning, FEMA had not accepted the request,” CBS studies. “DeSantis, in the meantime, mentioned he’s sending 100 nurses underneath contract with the state to Miami-Dade County.”
Some hospitals, notably in Miami-Dade County, are already dialing again on some elective procedures to minimize the pressure on workers and different assets. “The following step could be to declare surge capability — this really creates further capability by permitting a hospital to quickly cope with an emergency by doubling up affected person rooms and stress-free staffing ratios to exceed the hospital’s regular mattress depend,” he says. “You’ll be able to’t preserve that up for lengthy. A closing step could be to usher in area hospitals and important outdoors assets.”
On Monday, Senior warned Vox that he was fearful about hospitalizations exceeding 500 per day. “If day by day hospitalizations shoot up over 500 a day, there will probably be severe stress forward,” he says. “800 or 1,000 and it will likely be a wild journey.”
Sadly, the state is heading in that route. On Tuesday, Florida hit 533 hospitalizations:
:no_upscale()/cdn.vox-cdn.com/uploads/chorus_asset/file/20085299/Screen_Shot_2020_07_15_at_12.49.31_PM.png)
Tallahassee Stories/Florida Division of Well being
“If it grows exponentially from right here, there’s no denying, you realize, we’re gonna need to relook at every thing originally of August,” Senior notes.
Texas hospitals warn they’re working out of workers, PPE, medication, and different provides
Texas hospitals thought that they had already seen the worst of Covid-19 within the spring. This newest surge has surpassed that first surge a number of occasions over.
Through the first wave, from late February to early Could, Houston Methodist hospital peaked with about 250 coronavirus sufferers. At the moment, they’ve practically 700. “There are too many Covid sufferers, full cease,” Roberta Schwartz, government vice chairman at Houston Methodist, advised me. “We ran full earlier than, we’re working full-plus now.”
Their expertise mirrors the statewide tendencies: Hospitalizations in Texas had topped out at about 1,800 in early Could, however now, after circumstances started to speed up dramatically, they’ve surpassed 10,000.
“On daily basis, or each different day, we’re turning one other unit of this hospital into Covid items,” Schwartz says. “It’s slowly ravenous out the opposite providers that we provide.”
She ticked via the checklist: half a dozen of the hospitals’ medical surgical items are actually getting used to deal with Covid-19. An orthopedics unit has been shut down and flipped for sufferers who require high-oxygen circulation. Cardiology items have additionally shortened their surgical procedure schedules in order that their area can be utilized for the coronavirus surge.
Schwartz and John Henderson, president and CEO of the Texas Group of Rural and Neighborhood Hospitals, say their hospitals are in higher form now with private protecting tools than they had been in March and April.
However that might change because the disaster will get worse. Schwartz says her services have generally had bother getting robes and disinfectant wipes. Henderson says he “received a few SOS calls this week.”
Staffing is a common downside. Houston Methodist has already introduced in out-of-state nurses and requested its administrative workers with nursing certifications to begin doing medical work once more. Nurses are additionally being requested to work longer and in a single day shifts.
Rural hospitals in Texas aren’t working out of beds but, however they’re working right into a staffing scarcity. These services would possibly usually have 5 sufferers in a given unit, and the hospitals have staffed them accordingly. However now, there is likely to be as many as 20 sufferers.
“You’re working each nurse as a lot as you’ll be able to work them and nonetheless not assembly the necessity,” Henderson says.
It’s not clear the place extra workers might come from. The state has already despatched about 2,300 volunteers to the Rio Grande Valley, one of many hardest-hit areas within the state.
“Different areas are requesting that workforce help,” Henderson says. “However there’s not rather more by way of assets to be despatched.”
One other concern is ventilators. Rural hospitals in Texas would ordinarily switch their sufferers in severe situation, the sort who is likely to be on a ventilator for days, to a bigger hospital within the metropolis. However as a result of city hospitals are already overrun with Covid-19 sufferers themselves, there may be nowhere for the agricultural hospitals to ship their sufferers. As a substitute, they’re compelled to maintain these sufferers, inflicting their beds to refill much more rapidly.
And whereas the present coronavirus sufferers are youthful than these seen within the spring, Henderson says his hospitals don’t have sufficient of the nasal oxygen hook-ups which can be used to assist these sufferers breathe on their very own and forestall them from being placed on a ventilator.
“They’ve proven to be efficient however everyone’s making an attempt to get them,” he says.
Hospitals are placing classes from the early weeks of the disaster to make use of. Remdesivir, an antiviral therapy prescribed to Covid-19 sufferers with low blood oxygen or who want respiration help from a mechanical ventilator, is protocol now. The College Well being System in San Antonio, which received firsthand expertise within the preliminary wave when it was requested to deal with a number of the first sufferers from Wuhan and the Diamond Princess cruise ship, has tailored its customary of care to incorporate remdesivir, anti-inflammatory medication, and placing sufferers on their abdomen to assist them breathe. They’ve additionally lowered their use of ventilators, solely utilizing them when completely crucial.
However these enhancements in therapy require enough staffing and provides to implement them. And because the disaster grows, supples are beginning to run low.
“We nonetheless don’t have a gentle stream of sufficient remdesivir,” Schwartz at Houston Methodist says.
That’s the state of affairs on the bottom as of early July. Instances are persevering with to climb in Texas, and extra persons are anticipated to finish up within the hospital consequently. The emergency plan to arrange short-term services in conference facilities or sports activities venues is all of a sudden on the desk.
Hospitals like Memorial Hermann in Houston have already activated their surge capability plans, however that may not be sufficient if present tendencies proceed.
“We stay involved concerning the present progress fee in new circumstances and the demand for hospitalization, as we might attain the restrict of our surge enlargement plans if the present tendencies don’t reverse,” Drew Munhausen, a spokesperson for the hospital, says in an electronic mail.
The hope is that new circumstances will begin to stage off quickly, now that Gov. Greg Abbott has reimposed some social distancing restrictions and established a statewide masks mandate. However for now, Texas hospitals are simply ready and hoping and making ready.
“In case you’re counting hospital admissions and ICU sufferers on vents, you’re weeks behind. We’re chasing it proper now,” Henderson says. “There’s no optimism at this time for what the remainder of July appears like.”
The worst-case situation, in these moments, is that folks will die who in any other case wouldn’t have as a result of the scarcity of beds or provides or workers will result in suboptimal care.
Even worry itself will be devastating to public well being. As ProPublica and NBC Information reported, the variety of Houstonians dying at house has spiked in latest weeks, suggesting individuals who both had Covid-19 or one other life-threatening situation didn’t make it to the hospital in time.
“When you’re unable to handle sufferers within the optimum circumstances, you do fear that you’re not capable of do pretty much as good of a job in not-optimal circumstances,” Schwartz says. “And we’re about to get into not-optimal circumstances.”
It could possibly be a troublesome few weeks forward. Youyang Gu’s Covid-19 Projections at the moment expects circumstances in Texas to peak originally of August and deaths to peak in mid-August.
In Imperial County, California, a run on ventilators
El Centro Regional Medical Heart in Imperial County, considered one of California’s worst Covid-19 sizzling spots proper now, has already brushed up in opposition to its worst-case situation.
About 60 p.c of the sufferers within the medical heart had been contaminated with coronavirus as of final week they usually don’t have sufficient ventilators, Adolphe Edward, the hospital’s CEO, advised Vox. The medical heart serves a largely Hispanic group, with many sufferers who’ve diabetes or different preexisting situations that make them extra susceptible to the virus and who require mechanical ventilator help for his or her respiration when the illness takes a flip for the more serious.
The hospital lately noticed its accessible ventilators dwindle down to 1. Edward convened an impromptu committee to guage the sufferers at the moment on ventilators so they may prioritize if one other affected person who wanted one got here via their door. They checked their lung capability and thought of whether or not they might threat taking one or two of the sufferers off the ventilator if the necessity arose.
Fortunately, Edward found out a workaround. He known as one other close by hospital and requested if that they had any ventilators accessible. That they had two, which they shipped over to El Centro. For now, the machines are nonetheless there, although Edward says he and the opposite hospital have stayed in fixed contact in case the ventilators should be transferred once more.
Edward sounds exasperated describing that makeshift answer and he wonders why the federal authorities hasn’t began manufacturing “half 1,000,000 or 1,000,000” ventilators to satisfy the necessity that hospitals like his have.
“Any person’s gotta determine that out,” he says. (The Trump administration signed contracts in April underneath the Protection Manufacturing Act which can be speculated to yield rather less than 150,000 ventilators by the tip of 2020.)
Statewide, solely about 30 p.c of all accessible items are at the moment in use, in keeping with NPR. However there have been surges of sufferers in some areas like Imperial County which have practically overwhelmed native hospitals. About 30 p.c of ICU beds are nonetheless open statewide as nicely, however these numbers might begin shrinking because the state outbreak shifts from the youthful cohort much less vulnerable to severe issues to older people who find themselves extra more likely to require hospitalization and air flow.
A California plan to stockpile ventilators by no means really materialized, and the accessible capability could possibly be stretched with the hardest-hit areas exporting their sufferers to services in different elements of the state.
El Centro Regional Medical Heart is transferring sufferers out of its constructing at a fee Edward would ordinarily have discovered unfathomable. Throughout regular occasions, the hospital would possibly ship out one or two sufferers a day, he says. These days, they’re averaging between six and eight.
“In case you had advised me originally we’d be transferring that many sufferers, I’d have advised you: I don’t know what you’re consuming,” Edward says.
In the interim, hospitals elsewhere within the state have the additional area to accommodate them. However the fear is that if the outbreak retains spreading, that extra capability will evaporate in a short time.
New Covid-19 circumstances and deaths in California are at the moment anticipated to peak by August or early September, in keeping with Youyang Gu’s Covid-19 Projections, that means the brand new surge has not peaked but.
Extra hospitals could possibly be confronted with the sort of troublesome choices that Edward and his staff had been practically compelled to make.
Help Vox’s explanatory journalism
On daily basis at Vox, we goal to reply your most vital questions and supply you, and our viewers all over the world, with info that has the ability to avoid wasting lives. Our mission has by no means been extra important than it’s on this second: to empower you thru understanding. Vox’s work is reaching extra individuals than ever, however our distinctive model of explanatory journalism takes assets — notably throughout a pandemic and an financial downturn. Your monetary contribution won’t represent a donation, however it should allow our workers to proceed to supply free articles, movies, and podcasts on the high quality and quantity that this second requires. Please take into account making a contribution to Vox at this time.